Family describes anti-'sissy' therapy
STORY HIGHLIGHTS
- Siblings: Gay brother killed himself decades after treatment to make him more masculine
- Treatment included withholding maternal attention and punishment
- Ex-clinic psychologist: It's "inaccurate to assume" therapy caused Kirk Murphy's suicide
Editor's note: Tonight at 10 ET on CNN TV, "AC360º" examines a shocking "experimental therapy" designed to make feminine boys more masculine. See what one family says was the devastating result in a special report, "The Sissy Boy Experiment."
Los Angeles (CNN) -- Kirk Andrew Murphy seemed to have everything to live for.
He put himself through school. He had a successful 12-year career in the Air Force. After the service, he landed a high profile position with an American finance company
in India.
But in 2003 at age 38, Kirk Murphy took his own life.
A co-worker found him hanging from the fan of his apartment in New Delhi. His family has struggled for years to understand what happened.
 Gallery: UCLA's Gender Identity Clinic
Gallery: UCLA's Gender Identity Clinic "I used to spend so much time thinking, why would he kill himself at the age of 38? It doesn't make any sense to me," said Kirk's sister, Maris Murphy. "What I now think is I don't know how he made it that long."
After Kirk's death, Maris started a search that would uncover a dark family secret. That secret revealed itself during a phone conversation with her older brother Mark, who mentioned his distrust of any kind of therapy.
"Don't you remember all that crap we went through at UCLA?" he asked her. Maris was too young to remember the details, but Mark remembered it vividly as a low point in their lives.
IReport: Did you participate in similar research?
Wanting a 'normal life'
Kirk Murphy was a bright 5-year-old boy, growing up near Los Angeles in the 1970s. He was the middle child, with big brother Mark, 8, and little sister Maris, just a baby at 9 months. Their mother, Kaytee Murphy, remembers Kirk's kind nature, "He was just very intelligent, and a sweet, sweet, child." But she was also worried.
It left Kirk just totally stricken with the belief that he was broken, that he was different from everybody else.
--Maris Murphy, Kirk's sister
"Well, I was becoming a little concerned, I guess, when he was playing with dolls and stuff," she said. "Playing with the girls' toys, and probably picking up little effeminate, well, like stroking the hair, the long hair and stuff. It just bothered me that maybe he was picking up maybe too many feminine traits." She said it bothered her because she wanted Kirk to grow up and have "a normal life."
Then Kaytee Murphy saw a psychologist on local television.
"He was naming all of these things; 'If your son is doing five of these 10 things, does he prefer to play with girls' toys instead of boys' toys?' Just things like this," she said.
The doctor was on TV that day, recruiting boys for a government-funded program at the University of California, Los Angeles.
"Well, him being the expert, I thought, maybe I should take Kirk in," said Kaytee Murphy. "In other words, nip it in the bud, before it got started any further."
Kirk becomes 'Kraig'
Kaytee Murphy took Kirk to UCLA, where he was treated largely by George A. Rekers, a doctoral student at the time.
In Rekers' study documenting his experimental therapy (PDF), he writes about a boy he calls "Kraig." Another UCLA gender researcher confirmed that "Kraig" was a pseudonym for Kirk.
The study, later published in an academic journal, concludes that after therapy, "Kraig's" feminine behavior was gone and he became "indistinguishable from any other boy."
"Kraig, I think, certainly was Rekers' poster boy for what Rekers was espousing for young children," said
Jim Burroway, a writer and researcher who has studied Rekers' work.
I thought, maybe I should take Kirk in ... nip it in the bud, before it got started any further.
--Kaytee Murphy, Kirk Murphy's mother
"We have been wondering where is Kraig? A lot of us have talked about it. Where is he today? Is he married or is he gay? Or specifically does he even know that Rekers has been writing about him?" said Burroway. "I found 17 different articles, books, chapters, that he has written in which he talked about Kraig."
Rekers' work with Kirk Murphy helped him build a three-decade career as a leading national expert in trying to prevent children from becoming gay, a career as an anti-gay champion that would later be tainted by his involvement in an embarrassing scandal.
The experiments
The therapy at UCLA involved a special room with two tables where "Kraig's" behavior was monitored, according to the study.
"There was a one-way mirror or one-way window -- and some days they would let him choose which table he would go to," said Maris, who has read about the experiments.
At one table Kirk could choose between what were considered masculine toys like plastic guns and handcuffs, and what were meant to be feminine toys like dolls and a play crib. At the other table, Kirk could choose between boys' clothing and a toy electric razor or items like dress-up jewelry and a wig.
See details about the experimental therapy
According to the case study, Kaytee Murphy was told to ignore her son when he played with feminine toys and compliment him when he played with masculine toys.
"They pretty much told him he wasn't right the way that he was, but they never really explained it to him what the issue was. They did it through play," Maris said.
Rekers wrote that Kirk would cry out for attention, even throwing tantrums, but Kaytee Murphy was told to keep going.
Harsh beatings
At home, the punishment for feminine behavior would become more severe. The therapists instructed Kirk's parents to use poker chips as a system of rewards and punishments.
According to Rekers' case study, blue chips were given for masculine behavior and would bring rewards, such as candy. But the red chips, given for effeminate behavior, resulted in "physical punishment by spanking from the father."
Mark said he was told to participate in the chip reward-and-punishment system as a way to make Kirk feel like the system was OK.
I only meant to help, do the best I could with the parents.
--Dr. George Rekers
The family said the spankings were severe. Maris remembers "lots of belt incidents." She escaped the screaming by going to her bed to "lay in the room with my pillow on my head." Later, she would go to Kirk's bedroom and "lay down and hug him and we would just lay there, and the thing that I remember is that he never even showed anger. He was just numb."
During one particularly harsh punishment, their mother recalls, her husband "spanked" Kirk "so hard that he had welts up and down his back and on his buttocks."
She remembers her son Mark saying, "Cry harder, and he won't hit so hard." She says, "Today, it would be abuse."
Sometimes Mark would try to protect his brother, to make his beatings less severe.
"I took some of the red chips and I put them on my side," said Mark, as tears came to his eyes. But he said the beatings were still frequent.
The number of stacked red chips became a telltale sign about the level of tension in the house. When he returned home each day, Mark often looked for the chips in their easily visible location between the living room and the kitchen.
"You looked and were like, 'What's the chip count today? What happened? What changed? How bad is it going to be?' And it was always bad. There was whipping every Friday night. There was no way out of it."
Kirk's formal clinical treatment lasted 10 months, but the family said some of the treatment techniques and practices lasted longer at home.
'Different from everybody else'
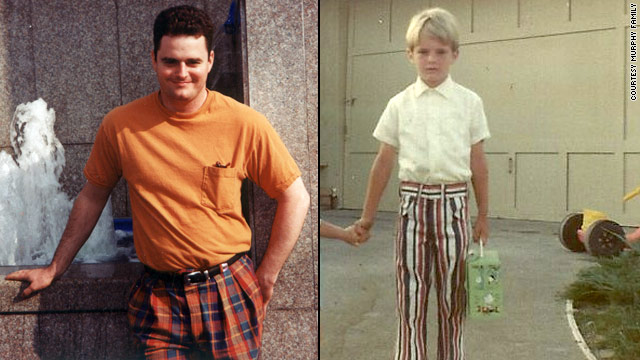
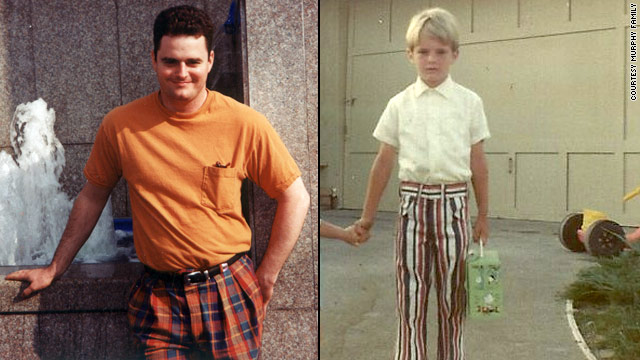
Mark Murphy vividly remembers a photo of a smiling young Kirk, age 4, taken a year before the therapy started.
"This is my brother, Kirk Andrew Murphy, right here," Mark said, pointing to the picture. "This is the way he's supposed to be right here," Mark said tearfully.
Mark said the photo shows the last time he remembers his brother as a happy child.
Maris, who was too young to remember Kirk when he went to therapy, said she only knew Kirk after his treatment.
"It left Kirk just totally stricken with the belief that he was broken, that he was different from everybody else," she recalled. "He even ate his lunch in the boy's bathroom for three years of his high school career, if you want to call it that."
CDC: Lack of acceptance can lead to risky behavior for non-straight youth
Kirk's mother said she believes the experimental therapy destroyed Kirk's life.
"I blame them for the way his life turned out," she said. "If one person causes another person's death, I don't care if it's 20 or 50 years later, it's the same as murder in my eyes."
Of course, the actual reason someone commits suicide is difficult, if not impossible to know. The family's allegations that Rekers' therapy caused Kirk Murphy to take his life are just that -- allegations.
When Rekers did not respond to CNN's repeated requests for an interview, CNN producers tracked him down in Florida to ask about the Murphy family's allegations.
It's "inaccurate to assume" therapy led to Kirk Murphy's suicide, says George Rekers, who treated Murphy.
"Well, I think, scientifically that would be inaccurate to assume that it was the therapy, but I do grieve for the parents now that you've told me that news. I think that's very sad," he said.
Rekers pointed out that the therapy had been decades earlier.
"That's a long time ago, and to hypothesize, you have a hypothesis that positive treatment back in the 1970s has something to do with something happening decades later. That would, that hypothesis would need a lot of scientific investigation to see if it's valid. Two independent psychologists with me had evaluated him and said he was better adjusted after treatment, so it wasn't my opinion." he said.
One of those psychologists has since died. The other -- Dr. Larry Ferguson -- told CNN that he did evaluate Kirk Murphy as a teenager. He said the family was well adjusted and he did not see any "red flags" when evaluating Kirk. But Maris Murphy says Kirk lied to those examining him. "He was conditioned to say what they wanted to hear," she said.
Rekers said he could not give specific details about Kirk Murphy's treatment, citing doctor-patient confidentiality. For him, the bottom line is that the therapy was intended to help.
"I only meant to help, do the best I could with the parents, and I've written articles you can look up, too, on the rationale for our treatment. And the rationale was positive; to help children, help the parents who come to us in their distress asking questions, 'What can we do to help our child be better adjusted?' " Rekers said.
Karl Bryant, a professor of women's and gender studies at the State University of New York at New Paltz, was also taken to UCLA as a child, as a part of a different study of effeminate boys.
Bryant said he thinks the more tragic part of Kirk's story is people "trying to do something good, trying to help ... even in a misguided mode, who end up producing these negative outcomes for people."
Bryant has studied the history of work done with children with opposite-sex behavior extensively, and said the studies are complex.
"I never have -- had tried to kill myself or thought that I was going to kill myself," said Bryant. "But I could identify with that pain of -- of feeling like you want to be something and other people want you to be something that you aren't."
'Unwanted homosexuality'
Rekers, who conducted the therapy on Kirk, went on to build a career of influence based on the premise from his research that homosexuality can be prevented.
He became a founding member of the Family Research Council, a faith-based organization that lobbies against gay-rights issues. Rekers was also on the board of the National Association for Research and Therapy of Homosexuality, an organization of scientists that
says its mission is to offer treatment to those who struggle with what they call "unwanted homosexuality."
"He's viewed as an expert by some, you know, when it's -- when it serves their purposes," said Bryant. "So, you know, basically, conservative and what I would call mostly 'fringe' groups have really, you know, Rekers as their poster boy."
Just last year, Rekers' days as an anti-gay champion would come to an end.
He hired a male escort to accompany him on his trip to Europe.
Rekers denies any sexual contact with the male escort. Rekers says he's not gay. He claims he wasn't aware that his companion offered sexual favors for sale over the Internet until after the trip, and says he hired him only to carry his bags. But the reporters who broke the story about Rekers' trip say they saw Rekers pushing a luggage cart through a Miami airport,
where they took his photo.
After the scandal broke, Rekers resigned from NARTH. And the Family Research Council said in a statement they hadn't had contact with Rekers in "over a decade."
Rekers vacations with 'rentboy'
His reputation among those who oppose homosexuality may be tarnished, but his research is still being cited in books and journals.
As recently as 2009, a book Rekers co-authored, "Handbook of Therapy for Unwanted Homosexual Attractions," cites Kraig's case as a success. That was six years after Kirk Murphy took his own life.
For Maris Murphy, there is more to the story than what was written in case studies about her brother.
"The research has a postscript that needs to be added," she said. "That is that Kirk Andrew Murphy was Kraig and he was gay, and he committed suicide."
"I want people to remember that this was a little boy who deserved protection, respect and unconditional love," his sister said. "I don't want him to be remembered as a science experiment. He was a person."
Journalists Penn Bullock and Brandon K. Thorp contributed to this report.